Ectopic Pregnancy
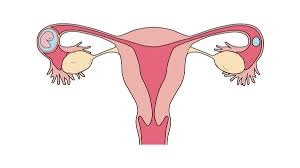
What the Disease Is
Ectopic pregnancy is a serious condition where a fertilized egg implants and begins to develop outside the uterine cavity, most commonly in one of the fallopian tubes. This type of pregnancy cannot proceed normally and poses significant health risks to the woman. The fertilized egg cannot develop properly in this location, and the growing tissue can cause severe complications, including tube rupture, internal bleeding, and potentially life-threatening situations. Prompt diagnosis and treatment are crucial to manage an ectopic pregnancy and preserve reproductive health.
Causes
- Fallopian Tube Damage: Damage or scarring of the fallopian tubes, often caused by pelvic inflammatory disease (PID), previous surgeries, or endometriosis, can disrupt the normal movement of the egg and result in ectopic implantation.
- Hormonal Imbalances: Abnormal hormone levels can interfere with the normal migration of the fertilized egg to the uterus, increasing the risk of ectopic pregnancy.
- Previous Ectopic Pregnancy: Women who have experienced an ectopic pregnancy in the past are at higher risk of having another.
- Contraceptive Use: While rare, certain forms of contraception, such as intrauterine devices (IUDs), can be associated with a higher risk of ectopic pregnancy if conception occurs.
- Assisted Reproductive Technologies (ART): Use of fertility treatments, including in vitro fertilization (IVF), may slightly increase the risk of ectopic pregnancy.
Predisposing Factors
- Pelvic Inflammatory Disease (PID): PID can cause scarring or damage to the fallopian tubes, increasing the risk of ectopic pregnancy.
- Endometriosis: This condition can cause pelvic inflammation and scarring, which may interfere with the normal function of the fallopian tubes.
- Previous Pelvic Surgery: Surgeries involving the reproductive organs can create adhesions or scarring that may lead to an ectopic pregnancy.
- Smoking: Women who smoke are at higher risk of ectopic pregnancy due to the effects of smoking on tubal function and reproductive health.
- Age: Advanced maternal age can be a factor, as older women are more likely to have preexisting conditions that increase the risk of ectopic pregnancy.
- Fertility Treatments: Some fertility treatments may alter the natural movement of eggs or embryos, increasing the risk of ectopic implantation.
Signs and Symptoms
- Abdominal Pain: Sharp or crampy pain on one side of the abdomen, which may be persistent or intermittent, is a common symptom.
- Vaginal Bleeding: Light to heavy vaginal bleeding or spotting, often different from a normal menstrual period, can occur.
- Shoulder Pain: Pain referred to the shoulder area, especially when lying down, can be a sign of internal bleeding and irritation of the diaphragm.
- Weakness or Dizziness: Symptoms such as weakness, dizziness, or fainting can indicate internal bleeding and may require immediate medical attention.
- Pelvic Pressure: A feeling of pressure or fullness in the pelvic region can be associated with an ectopic pregnancy.
Treatment and Management
- Medication:
- Methotrexate: This drug can be used to stop the growth of the ectopic tissue and is typically administered if the ectopic pregnancy is detected early and the tube has not ruptured.
- Surgical Intervention:
- Laparoscopic Surgery: Minimally invasive surgery is commonly used to remove the ectopic tissue and, if necessary, repair or remove the affected fallopian tube.
- Open Surgery: In more severe cases, open surgery may be required to address extensive damage or internal bleeding.
- Monitoring: Close monitoring through blood tests and ultrasounds is essential to ensure that the ectopic tissue is completely resolved and to manage any complications.
- Follow-up Care: Regular follow-up with a healthcare provider is necessary to monitor recovery, manage potential complications, and discuss future fertility options.
Prevention Strategies
- Avoiding Risk Factors: Reducing the risk of PID by practicing safe sex and getting prompt treatment for sexually transmitted infections (STIs) can help lower the risk of ectopic pregnancy.
- Regular Gynecological Check-ups: Regular visits to a healthcare provider can help identify and manage conditions that may increase the risk of ectopic pregnancy.
- Timely Management of Reproductive Health Issues: Early diagnosis and treatment of conditions like endometriosis and pelvic inflammatory disease can help prevent complications that may lead to ectopic pregnancy.
- Careful Use of Fertility Treatments: When undergoing assisted reproductive technologies, working closely with healthcare professionals to monitor and manage potential risks can reduce the likelihood of ectopic pregnancy.
Conclusion
Ectopic pregnancy is a serious condition that requires prompt medical attention due to its potential to cause significant complications, including life-threatening internal bleeding. Understanding the causes, symptoms, and treatment options is essential for managing this condition effectively. Early detection through regular gynecological care and addressing predisposing factors can help mitigate risks. By staying informed and seeking timely medical intervention, women can ensure appropriate management and preserve their reproductive health.